GERD (Gastroesophageal Reflux Disease)
Heartburn strikes everyone occasionally, but for millions, it's a recurring nightmare known as GERD (Gastroesophageal Reflux Disease). This chronic condition involves stomach acid persistently surging back into the esophagus, leading to irritation, discomfort, and potential long-term complications. Let's explore the science, the genetics, and the emerging research that could revolutionize GERD treatment.
The Mechanics of Mischief: How GERD Happens
At the heart of GERD is a malfunctioning lower esophageal sphincter (LES), a ring of muscle that acts like a gatekeeper between the esophagus and stomach. When working correctly, the LES allows food to pass down into the stomach but prevents acid from escaping back up. However, in GERD, the LES weakens, allowing acidic reflux to irritate the delicate lining of the esophagus.
Symptoms and Consequences: Beyond the Burn
While the hallmark of GERD is that burning sensation in the chest or throat (heartburn), it can manifest with a spectrum of other symptoms, including:
- Regurgitation
- Difficulty swallowing
- Chest pain
- Chronic cough
- Hoarseness
- Asthma-like symptoms
- Sore throat
If left untreated, GERD can lead to serious consequences, such as esophagitis (inflammation of the esophagus), ulcers, strictures (narrowing of the esophagus), and even a precancerous condition called Barrett's esophagus.
The Genetic Connection: Your DNA's Role in GERD
GERD isn't solely a lifestyle disease. Your genes play a significant part in your susceptibility. Numerous genes have been linked to GERD, including:
- FOXF1: This gene is essential for the development of smooth muscle in the digestive tract, including the LES. Variations in FOXF1 can affect the LES's function and increase the risk of GERD.
- MHC Genes: These genes regulate the immune system and inflammation, a key factor in GERD. Variations in MHC genes can influence the severity of inflammation in the esophagus.
- GNB3: This gene is involved in cell signaling, which affects how muscles contract. Variations in GNB3 can impact the LES's ability to close properly.
- Other Genes: Genes like CCND1 (associated with Barrett's esophagus), inflammatory cytokine genes (IL-1beta, IL-1RN), and DNA repair genes (COX-2, IL-10) have also been implicated in GERD.
Battling GERD: Medications and the Genetic Factor
A range of medications can effectively manage GERD, targeting different aspects of the condition:
- Antacids: These over-the-counter options neutralize stomach acid for quick relief.
- H2 Blockers: These reduce stomach acid production and are often used for mild to moderate GERD.
- Proton Pump Inhibitors (PPIs): These potent acid suppressors are commonly prescribed for frequent or severe GERD.
- Prokinetics: These medications help strengthen the LES and improve stomach emptying.
- Baclofen: This muscle relaxant can reduce the frequency of transient LES relaxations.
Interestingly, your genes can influence how your body responds to medications. For instance, variations in the CYP2C19 gene can affect how well certain PPIs are metabolized, potentially influencing their effectiveness and dosage.
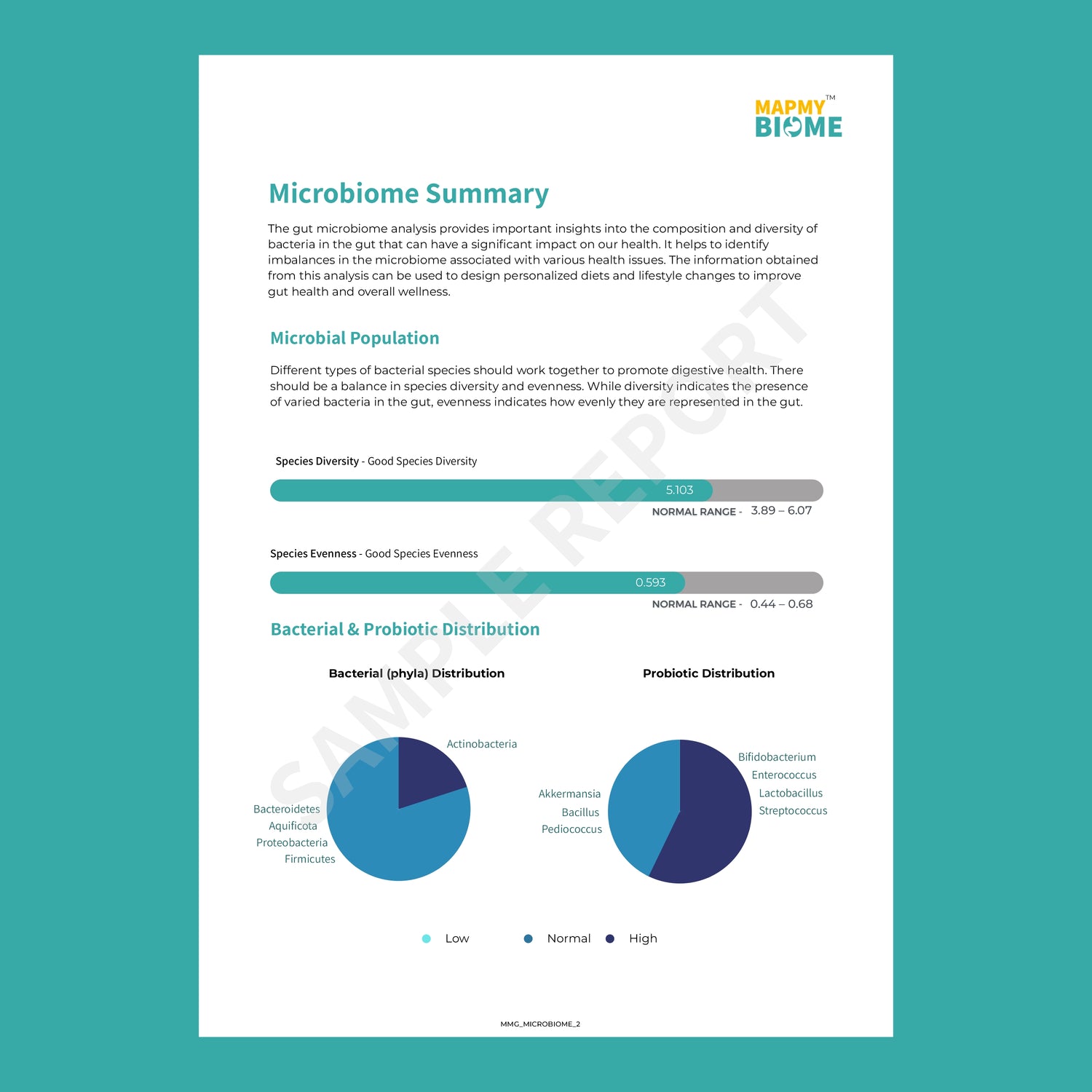
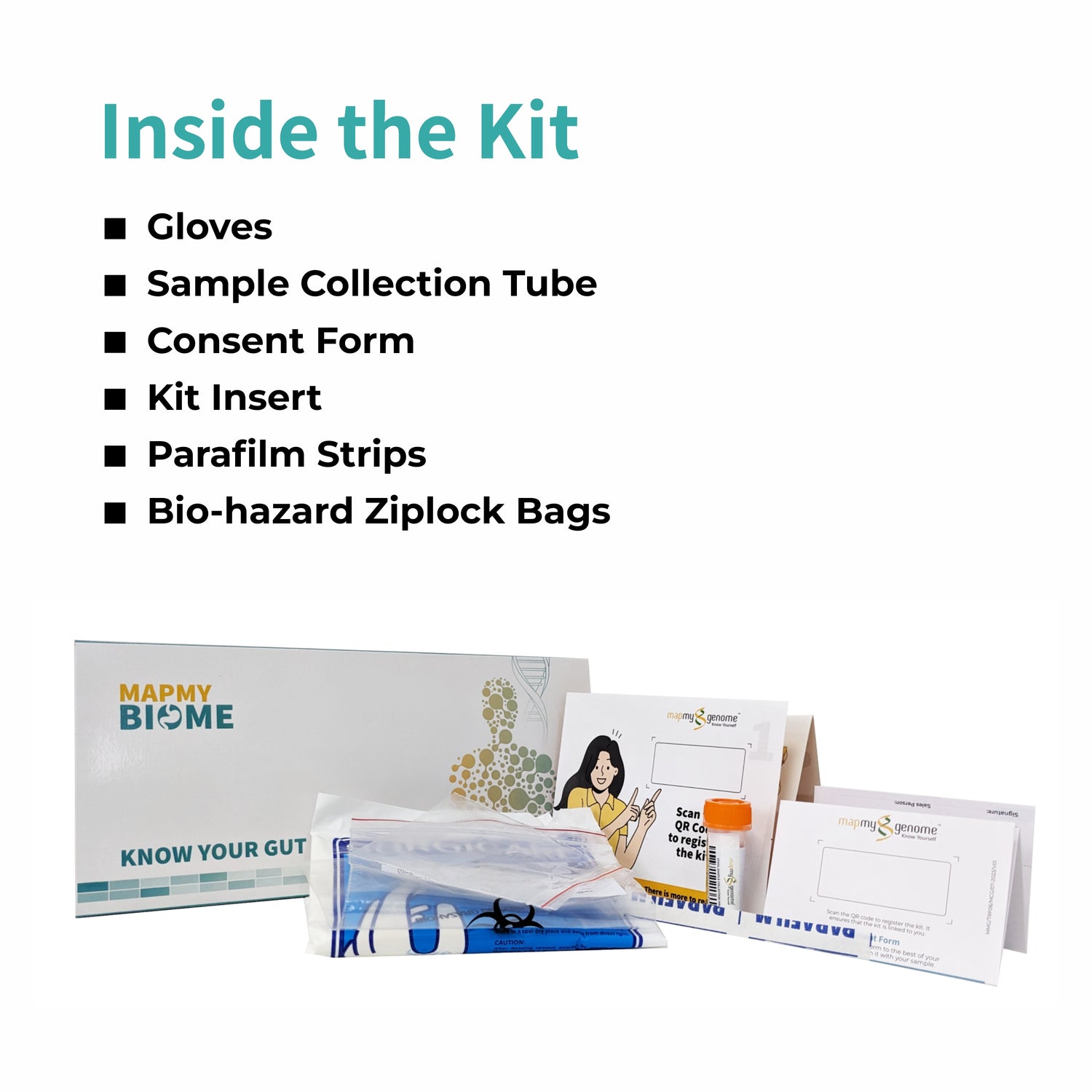
Gut Feeling: The Microbiome's Role in GERD
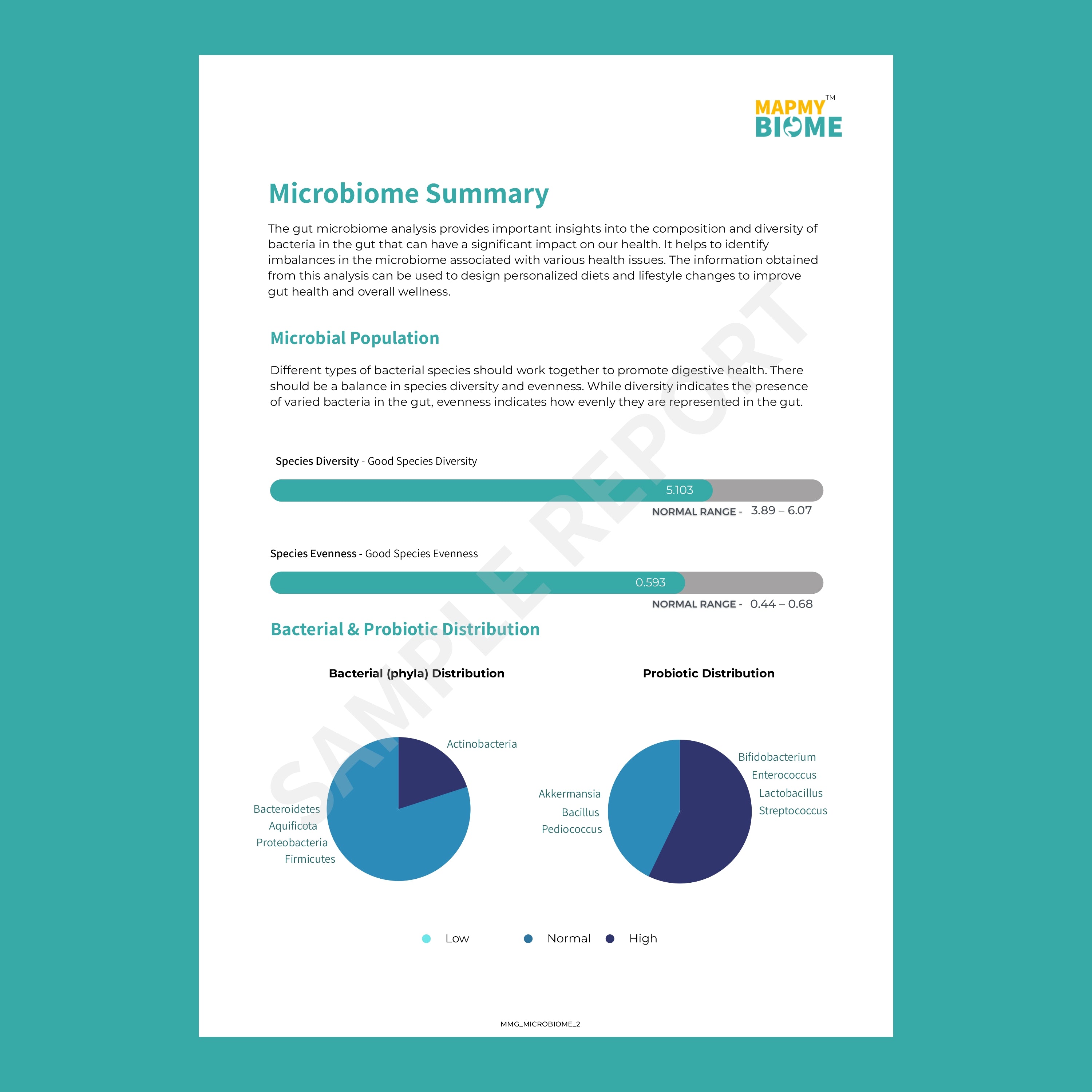
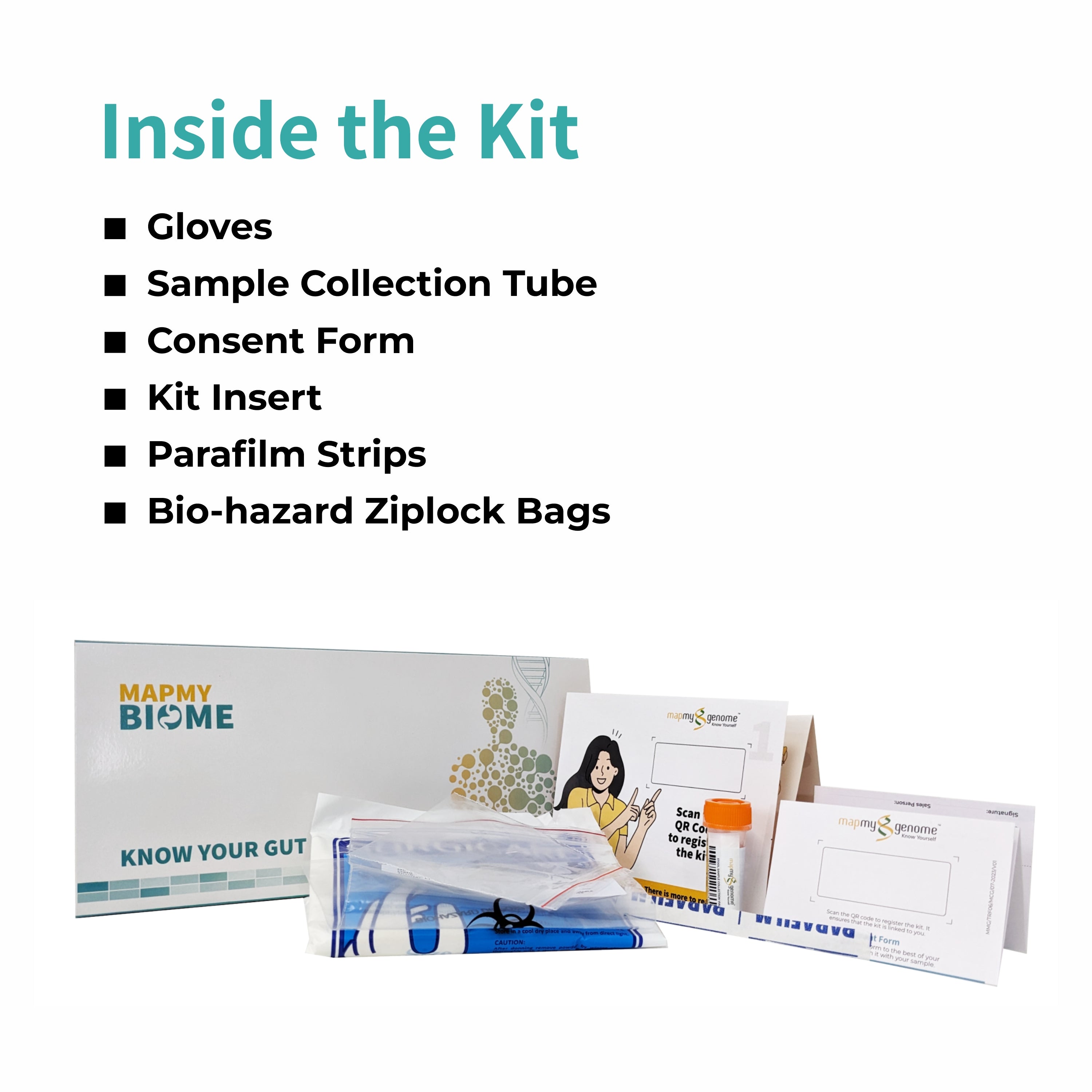
Emerging research suggests a fascinating link between the gut microbiome (the community of bacteria residing in our digestive tract) and GERD. Studies have shown that individuals with GERD often have a different microbiome composition than those without the condition.
Microbiome testing, which analyzes the types and amounts of bacteria in your gut, could potentially play a role in personalizing GERD treatment. Certain probiotics or dietary changes might be more effective for individuals with specific microbiome profiles. However, more research is needed to solidify the microbiome's role in GERD management.
Your GERD Action Plan
If you suspect you have GERD, don't hesitate to consult your doctor. They can assess your symptoms, medical history, and genetic predispositions to create a personalized treatment plan. This might include lifestyle modifications (e.g., dietary changes, weight management, avoiding trigger foods), medications, or even surgery in severe cases.
Remember, GERD is a multifaceted condition, and understanding the interplay of genetics, gut bacteria, and lifestyle factors is key to effective management. By staying informed and proactive, you can take control of your health and minimize the impact of GERD on your life.